Glucagon-Like Peptide-1 Receptor Agonists in People With Human Immunodeficiency Virus: An Expanded Meta-Analysis of Metabolic Outcomes
DOI:
https://doi.org/10.14740/cmmr114Keywords:
GLP-1 agonists, HIV, Weight loss, Antiretroviral therapy, INSTI, SemaglutideAbstract
Background: As a consequence of modern antiretroviral therapy (ART) regimens, people with human immunodeficiency virus (HIV) are disproportionately affected by weight gain and associated cardiometabolic comorbidities. Although glucagon-like peptide-1 receptor agonists (GLP-1 RAs) have emerged as efficacious weight loss modalities among the general population, little is known regarding the safety and efficacy among people with HIV undergoing treatment with ART.
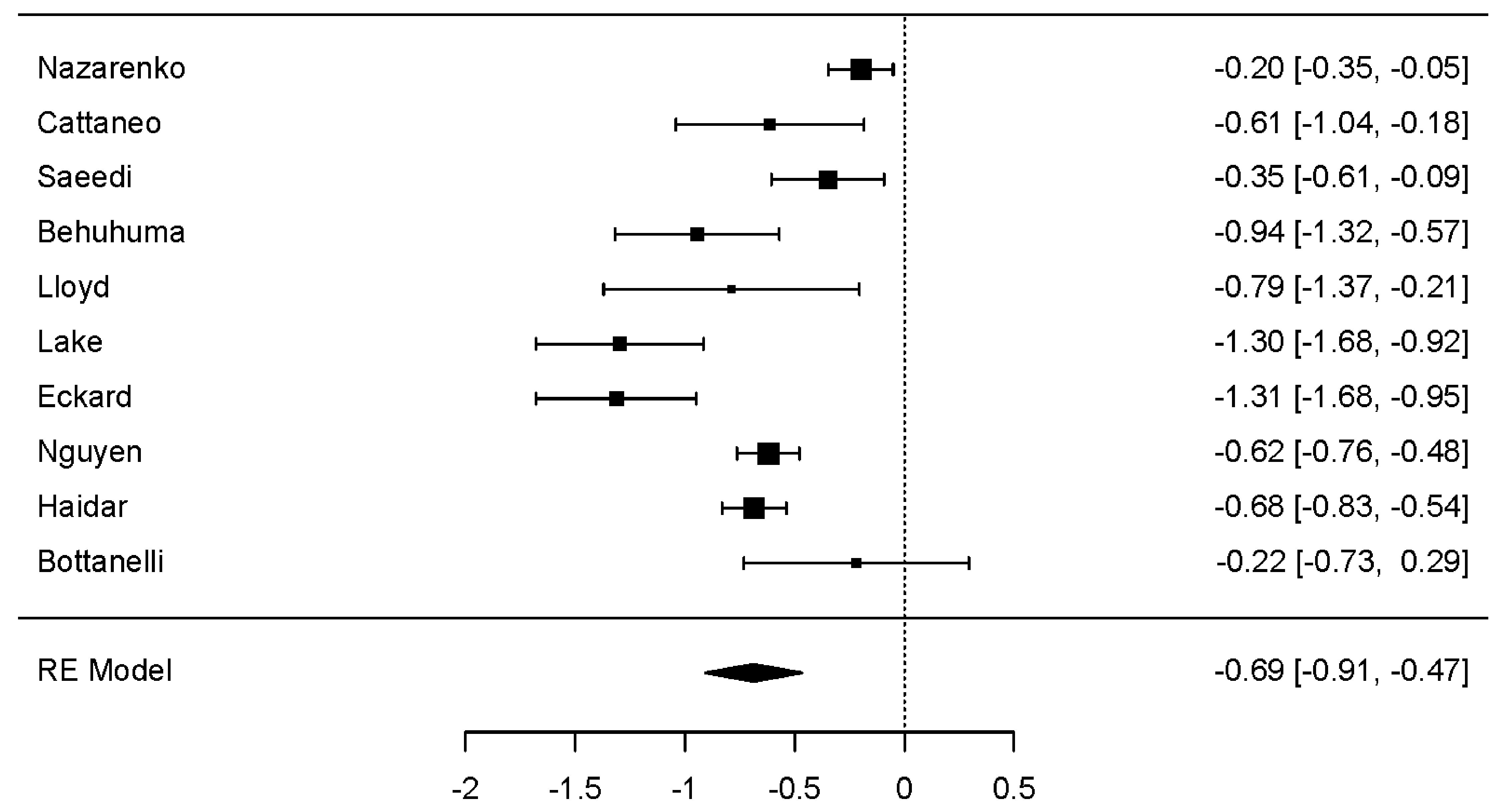
Methods: This study extended previous meta-analytic work evaluating the metabolic efficacy of GLP-1 RAs in people with treated HIV, due to a paucity of included studies under the initial protocol. A total of 10 studies, including both clinical trials and retrospective observational data, were analyzed to assess changes in weight, body mass index (BMI), and hemoglobin A1c (HbA1c). Meta-analyses were performed using random-effects models with robust analyses for heterogeneity and bias, as well as moderator analyses.
Results: GLP-1 RA use was associated with a statistically significant reduction in weight (d unbiased = -0.687, 95% confidence interval (CI): -0.908 to -0.467; P < 0.001), BMI (d unbiased = -0.693, 95% CI: -1.008 to -0.378; P < 0.001), and HbA1c (d unbiased = -0.539, 95% CI: -0.727 to -0.352; P < 0.001). Significant heterogeneity was observed across all outcomes, though publication bias was not consistently supported. Moderator analyses revealed greater weight and BMI reductions in clinical trials and in studies with a lower proportion of participants with type 2 diabetes (T2D). Dulaglutide use was associated with blunted effects across weight and BMI outcomes compared to semaglutide and liraglutide. Notably, semaglutide use did not yield significantly greater metabolic improvements relative to other GLP-1 RAs. Correlational analyses supported the role of T2D status and dulaglutide use in moderating treatment response. These findings align with existing data in the general population, where non-diabetic individuals and certain GLP-1 RAs (e.g., semaglutide) typically show greater efficacy.
Conclusions: Given the emerging concern around ART-induced weight gain and associated cardiometabolic risk, GLP-1 RAs may offer a promising therapeutic strategy in this high-risk population. Further research is needed to evaluate long-term safety, optimal agent selection, and patient-level predictors of treatment response.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.